A shorter treatment has been found for Multidrug-Resistant Tuberculosis (MDR-TB) after the conclusion of the World’s Largest clinical trial for the condition.
The results show both a fully-oral 9-month regimen and a 6-month injection-containing regimen to be safe and effective.
The two shortened treatment regimens for MDR-TB are also considered to be in lower costs to patients, according to officials.
The report published in The Lancet, was revealed during the opening of the Union World Conference on Lung Health 2022 (WCOLH) ongoing virtually.
Results from the trial is critical at this time when the world is witnessing an increase in TB cases and deaths.
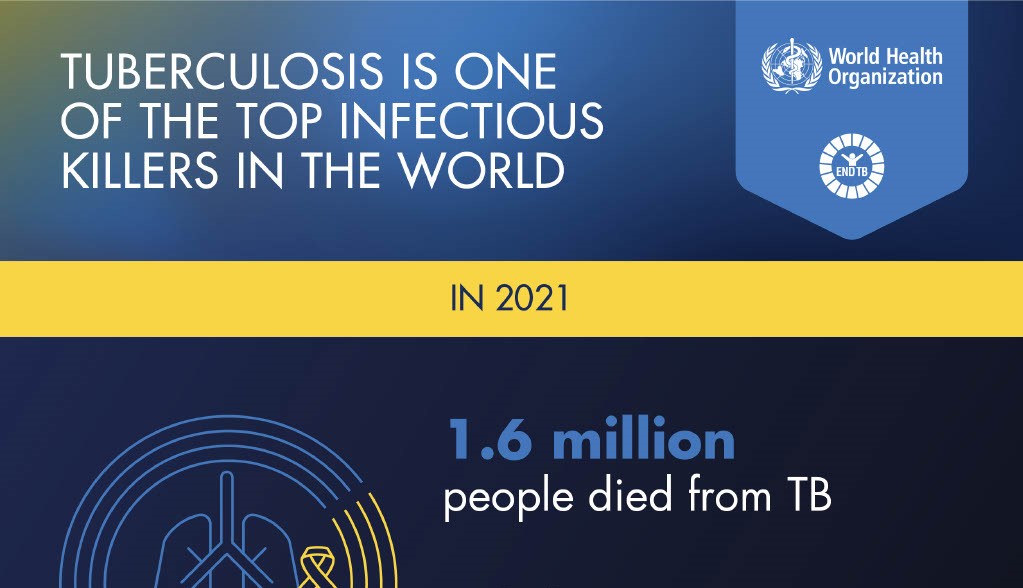
The 2022 Global TB report by the World Health Organisation estimated that 10.6 million people fell ill with tuberculosis (TB) in 2021, a 4.5 percent increase from 2020.
1.6 million people died from TB which included 187 000 among HIV positive people.
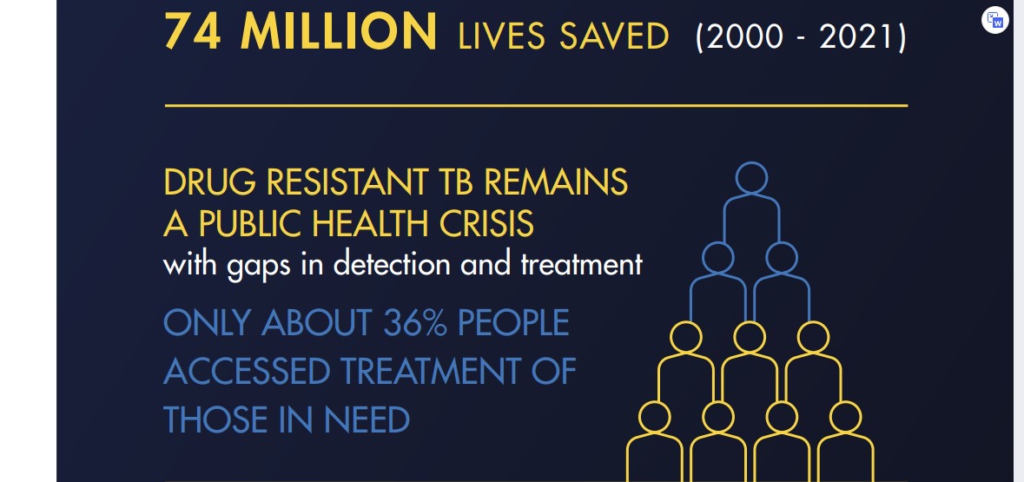
Cases of Multidrug-resistant TB (MDR-TB) also increased by 3.1 percent between 2020 and 2021, with 450 000 new cases of rifampicin-resistant TB (RR-TB) in 2021.
President of The Union and convenor of the WCOLH, Guy Marks said, “In the most recent data there has been an increase, both in the incidence and number of people dying due to tuberculosis. What this means is that there is real urgency about trying to turn around this epidemic.”
The MDR-TB Clinical Trials
The STREAM Clinical Trial is the world’s largest MDR-TB trial ever conducted with over thousand (1,000) participants recruited from eight countries on three continents.
Two stages of the STREAM trials have been done so far under the WHO regimen guidelines.
Stage 2 evaluated two new regimens – an all-oral 9-month regimen and a 6-month injection-containing regimen – both containing the new anti-tuberculosis drug bedaquiline – compared to a 9-month control regimen studied in Stage 1.
The research was built on the findings from Stage 1 of the STREAM trial, which demonstrated that a 9-month regimen that contained injections but did not contain bedaquiline was non-inferior to the 20-24 month regimen recommended in the 2011 WHO guidelines at the time the trial began.
Mr Marks said these results are very encouraging for the thousands of people affected by MDR-TB.
“Increased effective treatment options, means better choices for people with TB, which ultimately improves treatment outcomes and quality of life.”
The Results
It revealed that the fully-oral 9-month regimen was more effective than the 9-month control regimen; 82.7 percent of participants receiving the fully-oral regimen had a favourable outcome compared to 71.1 percent receiving the control regimen.
It also showed that the 6-month regimen which contained bedaquiline and an injectable medicine for an abbreviated period of two months- was also more effective than the control regimen; 91 percent of participants receiving the 6-month regimen had a favourable outcome compared to 68.5 percent in concurrent controls.
Reducing patient costs is important to eliminate catastrophic costs for TB-affected families, as targeted by the World Health Organization.
There was a within-trial health economics study led by the Liverpool School of Tropical Medicine that found that the fully-oral treatment is more expensive than the control regimen from a health system perspective –largely driven by the cost of the regimen; however, patient direct costs were lower in both study regimens compared to the control regimen.
Senior Vice President, Vital Strategies, and Sponsor for the STREAM trial, I.D. Rusen, explained that, “In STREAM Stage 2 we generated robust scientific evidence regarding the safety, efficacy, and cost-effectiveness of two shortened regimens for MDR-TB, providing guideline development groups and national TB programs with better information to underpin their decisions about the most appropriate treatments for their populations.”
The trial was sponsored by Vital Strategies and implemented with global partners, including the Medical Research Council Clinical Trials Unit at the University College London (UCL), the International Union Against Tuberculosis and Lung Disease (The Union) and Liverpool School of Tropical Medicine.





